Dental Implant Considerations
Dental Implants can be highly predictive if properly planned. There are many issues that need to be considered within the full assessment of implant planning. Below are keys points that may lead to the failure of an implant to integrate into the bone.
- Aged
- Older Individuals (Elderly) -> Delayed Healing
- Medical conditions are potential risk factors for surgery and also predispose to poor healing and potential non-union.
- Cancer, HIV, Cardiac disease, Blood dyscrasia, anticoagulant, mental health issues, uncontrolled acute infections, uncontrolled diabetes, irradiation of the jaw.
- Surgical Issues
- Placement
- Technique Sensitive
- Size of space – At least 6mm width or 3mm from adjacent structures, if this biological limit is not satisfied, there is a risk of ischaemia to the tissues, potentially leading to non-union.
- Height of space – An implant will not integrate into areas of non-bone. Eg sinus, IAN nerve
- Improper placement – Perforation through the cortical plate.
- Material
- If the implant is not osseoconductive with bone, it is unlikely to integrate
- Titanium, zirconium, ceramics, hydroxyapatite
- Protocol
- Heat – A temperature in excess of 47C during implant surgery can result in cell death and denaturation of collagen; as a result osseointegration (OI) may not occur (instead the implant may become surrounded by a fibrous capsule and the shear strength of the implant host interface is significantly reduced). Drill speed, design, amount of bone removed, and cooling are all considerations.
- Contamination
- Organic and inorganic debris can prejudice the achievement of OI. Materials such as necrotic bone, bacteria, chemical reagents and debris from the drill can be harmful. Also, like with like must be remembered. If the titanium interface for example is touched with steel for example this may contaminate the surface, increasing the potential for non-union.
- Stability
Dental Implant Considerations
- If primary stability is achieved (initial fit), the implant is more likely to integrate (Secondary stability)
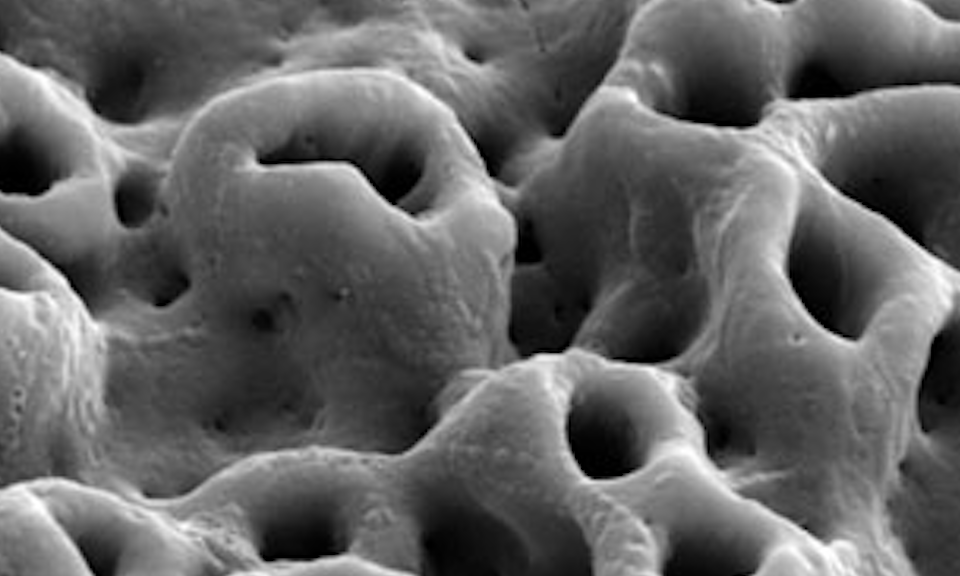
- This is related to the size of the implant but also the site, in terms of quality, fit, shape and bone morphology and density.
- If the bone is soft with large marrow spaces and sparse cortices, this provides a less favourable site to achieve primary stability (Some implant designs are oversize or self-tapping to overcome this issue.
- Bone quality
- A function of bone density, anatomy, and volume. Cawood and Howell Classification (relates to the amount of reporting)
- If the volume is an issue, smaller implants may need to be placed -> may result in overloading -> potentially leading to failure.
- Loading
- Early
- There is good research evidence that high initial loads on an implant immediately following placement result in the formation of a fibrous capsule rather than OI.
- On the other hand, there is evidence to suggest that if primary stability is ok, OI may still occur with early loading.
- Late
- Extensive mechanical loads on the implant can result in the breakdown of the interface with resultant implant failure. It is generally considered that overloading should be avoided. This could arise as a result of bruxism / or superstructure designs / with the result of excessive cantilevering designs causing excessive forces.
- Early
Finally, If you wish for more information on dental implants please do not hesitate to contact Skygate Dental today at (07) 3114 1199 or 0406 579 197.